She's So Hysterical!
The "Science" and
History of Female Hysteria: A Wild Diagnosis, But Even WILDER Treatment
In terms of strange or bizarre historical
diagnoses in women's health, that of "Hysteria" may top the list. No
longer recognized as a true medical disorder today, female hysteria was a once
common medical diagnosis for a variety of female ailments – both physical as
well as psychological. Oddly enough, we still use the term
"hysterical" in our modern day vocabulary:
"Did you see such and such movie? It was
hysterical!"
Or
"She was so hysterical after she failed the
test we could not even reason with her."
However, if we trace back both the meaning and the
treatment of this common day verbiage, we may be more hesitant to use it in our
daily dictum.
Historical Perspective
Egyptian
You may be surprised to know that the first
description of the condition of hysteria dates back to ancient Egypt circa 1900
BC. This disorder of emotional state was thought to originate from spontaneous
movement of the uterus within the female body. References to this condition can
be found in the ancient medical treaties, the Kahun Papyri. These ancient
Egyptian text describe the variety of mathematical and scientific topics. Most
of these texts can be dated to circa 1820 BC.
Among the oldest of these documents (1600 BC) a
remedy for symptoms of depression related to hysteria can be found. Due to the
"wandering uterus theory", therapies varied based on where the uterus
was thought to reside. For example, if the uterus had "floated"
towards the head, the patient may be treated by placing malodorous herbs by the
nostrils thereby forcing the uterus back down towards the pelvis.
Alternatively, if uterus had fallen to low in the pelvis, acrid herbs to be
placed near the vaginal entrance in order to drive the misplaced uterus
cephalad.
Greeks
The term hysteria can be traced back to the great
physician Hippocrates (5th century BC). Based upon historical writings, is
evident that he also believed in the "wandering nature" of the
uterus. In fact, the term is taken from the Greek word for uterus, hyst.
in his collection of medical writings, the Hippocratic corpus, a variety of
systematic irregularities are described supposedly caused by the movement of
the woman's uterus. One exert recommends pregnancy to cure such symptoms. As
described therein, intercourse would "moisten" the womb and
facilitate blood circulation within the female body.
Rome
Claudius Galenus (2nd Century AD) also sought to
elucidate this mysterious female ailment. Galenus was a prominant Greek
physician, surgeon and philosopher in the Roman Empire. In one of his
written treatises, Galen describes his findings:
"I have examined many hysterical women, some
stuporous, others with anxiety...the disease manifests itself with different
symptoms, but always refers to the uters". Galenus' proposed treatments
for hysteria included purgers, administration of herbs, and sexual
release following marital arrangements.
Middle Ages
During the middle ages, doctrinal teachings of
Hippocrates and Galen continued to be propagated. A chief advocate for
women's health in the Middle Ages was surprisingly, a female physician.
Trota de Ruggiero (11th Centry AD). Trota is considered the first female
doctor in Christian Europe.
Trota (as known as Trota of Salerno) was born around 1090 AD, and was a student
at The Scoula Medica Salernitana- which many scholars believe was the first
medical school in the Western World. It was among the first to allow female
students into the study of the healing arts. In devoting
herself to women and their particular medical needs, she was arguably the first
gynecologist, and advocate for women's healthcare. She is known for having
written two important works on women’s' health and even commented on the
nature of hysteria. The medieval medical writings of Trotula blamed
the disease on "the retaining of blood or of corrupt and venomous uterine
humors that should be purged in the same way that men are purged of seed."
During the late Middle ages (1500-1700s), the supernatural provided theories of
its own. The "Malleus Maleficarum" (Latin for "The Hammer
of Witches") was a popular and famous book on witches and evil in the time
period. This book called the uterus the source of evil, and hysteria
ceased to be a physical disease to become a supernatural one. Prayers,
incantations and exorcism were suggested, as well as protective amulets, to
cure the possessed and protect the pure. Torture and executions were often
carried out as well.
However, the Greeks and Romans had already claimed that hysteria was linked to the
uterus and sex, and these beliefs were reintroduced during the Middle Ages as
more Ancient texts became available, thus changing the perception of hysteria
from a supernatural (demonic) disease to a physical one. Based on the
translations of Hippocrates's and Galen's texts from Ancient Greek and Latin
into Arabic, which were in turn translated back into Ecclesiastic Latin, it was
determined that the womb, an not demons, was the source of the ailment.
Victorian Era
According to the published work by Rachel Maines
(The Technology of Orgasm: "Hysteria", the Vibrator, and Women's
Sexual Satisfaction), hysteria was the second most common diagnosis in women
after fevers. Its presence was defined by a constellation of symptoms-anxiety,
nervousness, pelvic pain, erotic fantasies, and even fainting. Another theory
was proposed in addition to that of the wondering uterus in the 17th century.
The condition was believed to result from uterus "choking" the
patient because of unexpended seed caused by sexual deprivation. Women
with hysteria were encouraged to marry quickly or were not possible, engage in
activities such as horseback riding or the use of "female swings" to
aid in relieving the deprivation.
Homas Sydenham, an influential British physician
(mid- to late-1600s) wrote that these afflicted ladies were wandering
around ubiquitously. Sydenham once declared that female hysteria -- which he
attributed to "irregular motions of the animal spirits"- was the most
common cause for female dysfunction.
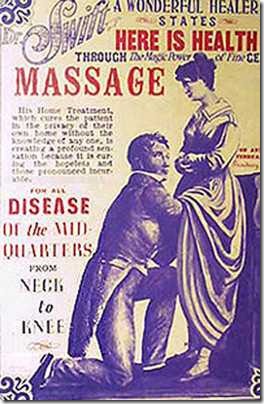
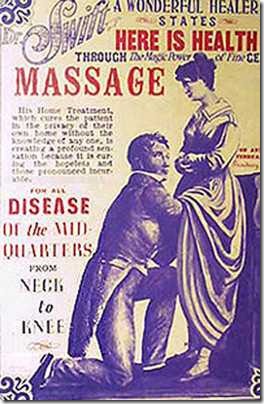
Treatments
One of the earliest records of treatment originates by Galen (2nd
Century). As Galen believed the root cause to be female sexual frustration,
most of his proposed therapies had to do with marriage and sexual
intercourse. For the virgins or widows, he
prescribed “pelvic (genital) massages” until “release” occurred. His techniques
would be cited by physicians for centuries to come. During the 1100s, in
addition to marriage and pelvic massage, irritating suppositories and fragrant
salves were suggested as treatment. The twin treatments of marriage or pelvic massage
continued into the Renaissance era. In the mid 16th Century, French
surgeon Ambroise Paré continued to encourage pelvic massage as the panacea for
hysteria, and as expressed in his sixteenth century text, married women should "bee
strongly encountered by their husbands” to have release. As an adjuvant
therapy, some began to advocate “water massage” of the pelvis for those not
responsive to traditional techniques. By the mid-1800s, spas
throughout Europe and the United States offered the "douche"—a spray
of water directed at the pelvic area—as a treatment that, according to one
writer in 1851, seemed to especially "commend itself to the ladies." British
observer Therme Malvern in 1851 wrote that after "hydrotherapy" women
were happy as if "they drank champagne."
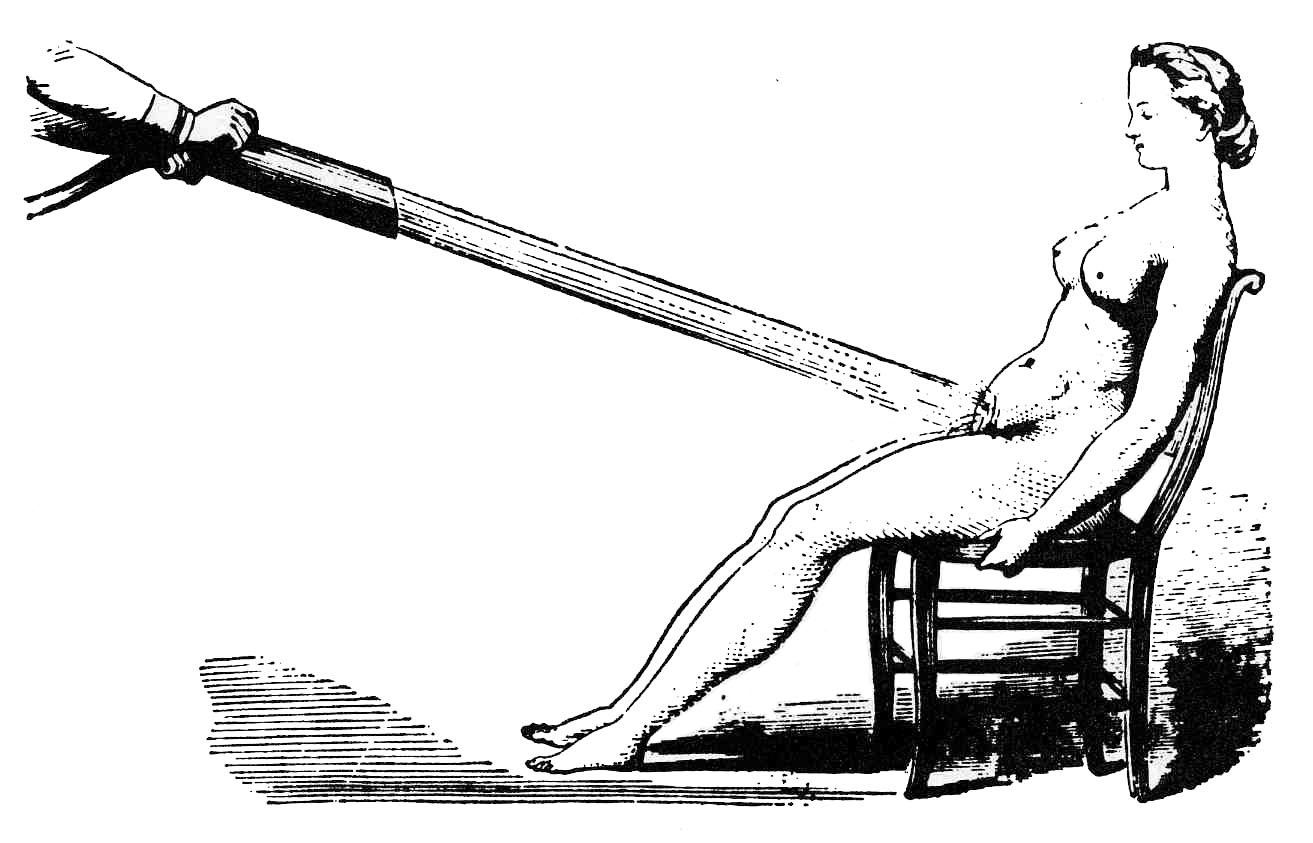
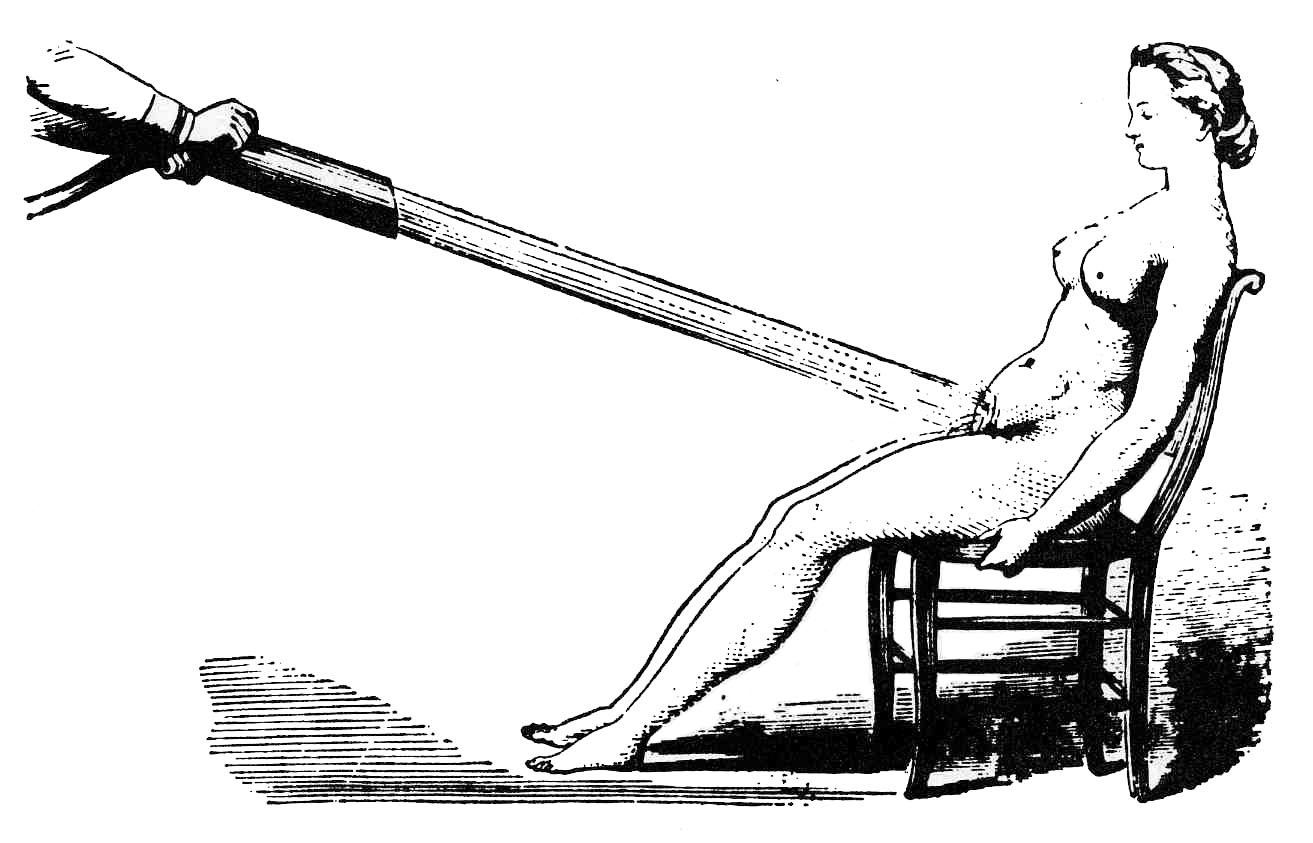
Water
massages as a treatment for hysteria (c. 1860)
These "pelvic massages" were to be performed manually, until the patient reached a "hysterical paroxysm", after which she appeared miraculously restored. The pelvic massage was a highly lucrative staple of many medical practices in 19th-century London, with repeat business all but guaranteed. There is no evidence of any doctor taking pleasure from its provision; on the contrary, according to medical journals, most complained that it was tedious, time-consuming and physically tiring. However, historical reports do describe ladies enjoying the therapy. Wealthy women from the higher strata of society regularly visited their personal physicians. The massage was administered once a week, sometimes doctors have resorted to alternative procedures for stimulation. This being the Victorian age of invention, the solution was obvious: devise a labour-saving device that would get the job done quicker, and perhaps, more discretely. What ensued next…yes, you guessed it.
 The first electric vibrator hit the scene in the late 1800s, which decreased treatment times from as much as an hour to as little as 10 minutes. George Taylor, an American doctor, patented the first steam-powered vibrator in 1869. A far cry from its sleek, portable successors, the "Manipulator" was a large and cumbersome table with a cut-out for a vibrating sphere. While Taylor recommended using his device to treat pelvic disorders, he warned that women should be supervised to prevent "overindulgence." This bulky
and expensive device was mounted under a couch, and equipped with a slot where
women would lay for a treatment. 14 years later (1883), his British
counterpart, Joseph Mortimer Granville, invented a more compact and
user-friendly electric version of the device: a drill with a small ball on the
end. When clicking on the device, it would start humming. The electric power
was supplied from the battery the size of a suitcase. The rest, as they say, is
history.
The first electric vibrator hit the scene in the late 1800s, which decreased treatment times from as much as an hour to as little as 10 minutes. George Taylor, an American doctor, patented the first steam-powered vibrator in 1869. A far cry from its sleek, portable successors, the "Manipulator" was a large and cumbersome table with a cut-out for a vibrating sphere. While Taylor recommended using his device to treat pelvic disorders, he warned that women should be supervised to prevent "overindulgence." This bulky
and expensive device was mounted under a couch, and equipped with a slot where
women would lay for a treatment. 14 years later (1883), his British
counterpart, Joseph Mortimer Granville, invented a more compact and
user-friendly electric version of the device: a drill with a small ball on the
end. When clicking on the device, it would start humming. The electric power
was supplied from the battery the size of a suitcase. The rest, as they say, is
history.
Late 19th Century
A more modern understanding of hysteria as a psychological disorder was
advanced by the work of Jean-Martin Charcot, a French neurologist. This
provided a shift to a more modern psychological view of hysteria. This was
expanded later by Sigmund Freud. By the 1920s, Freudian psychoanalytic theory
attributed hysterical symptoms to the unconscious mind's attempt to protect the
patient from psychic stress. The birth of “modern” psychoanalytic theory had
occurred. And so began the deterioration of the once popular diagnosis once
thought to plague up to 75% of women in the Victorian Age, Hysteria.
Myth vs
Medical Innovator
Lore describes the tale of Cleopatra (69-31 BC) as having the original
idea that resulted in the first vibrator (a hollow gourd full of angry bees (
for her personal pleasure. Whether this was true or not, we may never know.



.jpg)